Why Infrastructure Will Define the Future of Radiology AI
A System at Breaking Point
Healthcare costs are climbing faster than economies can bear. In radiology, the pressure is acute: demand for imaging rises year after year, while staffing levels lag far behind(1). The result is burnout, delays, and growing diagnostic errors(2).
Patients feel this directly. In the UK, fewer than one in four patients are satisfied with NHS care(3)(4). Waiting lists stretch for months, while radiologists face overflowing worklists. Despite massive spending, outcomes continue to disappoint.
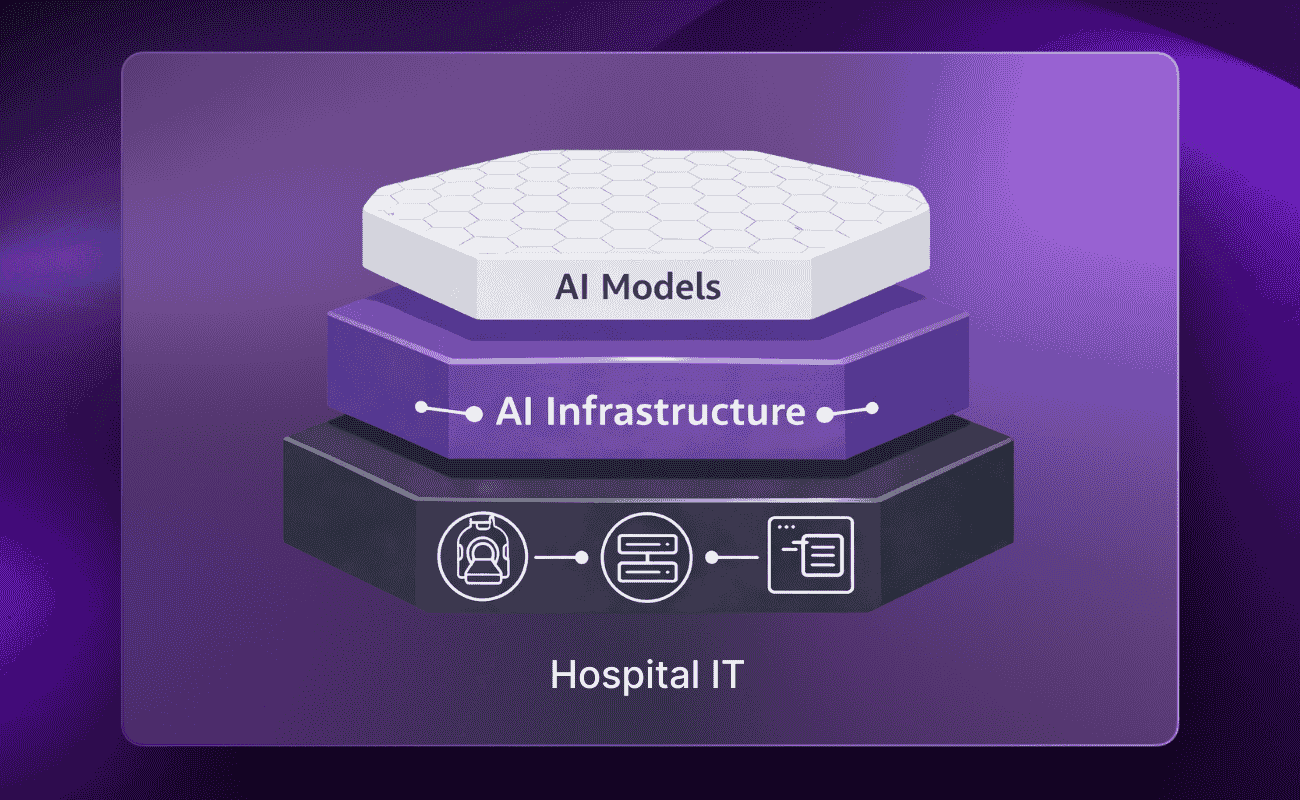
AI is often presented as the solution. But without strong infrastructure, even the most advanced models cannot deliver at scale(5). Infrastructure—not algorithms alone—will define the next decade of radiology
Data: The Real Currency of AI
Hospitals generate more data than ever: imaging, lab results, electronic records, and even genomics. This data holds immense value, but much of it remains siloed, inconsistent, and inaccessible.
AI models thrive on rich data. Early algorithms tackled one scan for one task. Today’s foundation models can span multiple organs, modalities, and even link imaging with biomarkers(7). The potential is extraordinary, but only if hospitals can securely access and govern their data.
Validation must also happen locally. Benchmark results elsewhere matter little if an algorithm fails on your patient population(6). Infrastructure must make side-by-side comparisons and a safe, real-world testing routine.
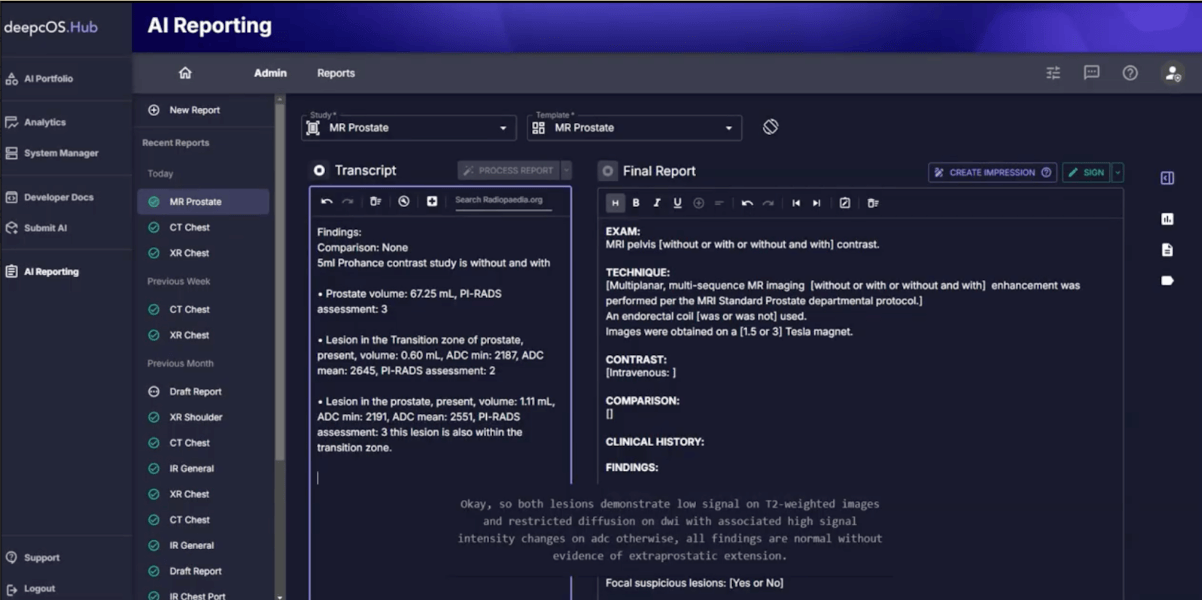
Infrastructure Platforms, Not Point Solution
Point solutions create fragmentation. Every new tool adds integration costs, governance reviews, and ongoing maintenance. Hospitals cannot scale if they juggle dozens of disconnected apps.
Infrastructure platforms offer a better way. They centralize deployment, monitoring, quality control, and compliance in a single place. They make ROI visible and workflows sustainable. Crucially, infrastructure platforms can remain vendor-neutral, linking diverse EHRs, PACS, and RIS systems without locking hospitals into a single ecosystem.
This neutrality builds trust. Hospitals retain flexibility, scale faster, and avoid the dead ends of one-off solutions.
Governance Builds Trust
Adoption is not only about performance. It is about safety, accountability, and trust. Without oversight, models drift, bias emerges, and liability grows.
Infrastructure must embed governance from the start: audit trails, privacy safeguards, regulatory alignment, and post-deployment monitoring. Standards like DICOM, FHIR, and OMOP enable interoperability across systems(8). Shared accountability between hospitals, vendors, and distributors ensures responsibility is clear and risks are managed(9).
Governance is not bureaucracy: it is the foundation of trust. Without it, clinicians hesitate to rely on AI, and adoption stalls.
People and Incentives Matter Most
Technology alone does not drive adoption. Hospitals already juggle years-long IT roadmaps and scarce resources. For staff, new AI tools often feel like just another burden.
Three factors make the difference:
- Clinical champions who push projects forward inside hospitals.
- Incentives that go beyond vague cost savings and show direct value.
- Patient engagement that frames the real choice: wait months for a human specialist or receive timely AI-assisted care today.
When framed honestly, patients and clinicians alike recognize the urgency. Change happens not through technology alone, but through people who clearly see its benefits.
Conclusion
Radiology is reaching a tipping point. Rising costs, limited staff, and growing demand leave no room for delay. AI has the power to help, but only if supported by robust infrastructure.
Hospitals equipped with AI infrastructure—neutral, scalable, and governed—will unlock the real value of AI. Those who cling to fragmented tools risk falling further behind. Algorithms will not define the future of radiology, but will be defined by the systems that allow them to work.
To hear how leaders are already tackling these challenges, watch the full webinar on radiology AI infrastructure.
Reference
- The Royal College of Radiologists (RCR). (2024). Clinical Radiology Census Report 2023.
- Medscape. (2024). Physician Burnout & Depression Report 2024.
- Nuffield Trust. (2024). Public satisfaction with the NHS sinks to a new record low.
- The King's Fund. (2024). Public satisfaction with the NHS and social care in 2023.
- Strohm, L., et al. (2022). Implementation of clinical artificial intelligence in radiology: who decides and who is responsible? Insights into Imaging.
- Yu AC et al: External Validation of Deep Learning Algorithms for Radiologic Diagnosis: A Systematic Review. 2022
- Bian, Yueyan et al. “Artificial intelligence in medical imaging: From task-specific models to large-scale foundation models.” Chinese medical journal vol. 138,6 (2025)
- Sengupta, A., et al. (2024). Integrating and Adopting AI in the Radiology Workflow: A Primer for Standards, Regulations, and Reference Architectures.
- The Royal College of Radiologists (RCR). (2024). AI deployment fundamentals for medical imaging.


.png)
.png)