The Radiology Report: 125 Years of Fascinating History
Explore the origins of the radiology report, how they have changed through time as well as what could be in store for the future.

In1895, Wilhelm Konrad Röntgen discovered X-rays, almost by accident, in his laboratory in Germany. Within less than one year after publishing his discovery in a paper called “On a New Kind of Rays,” the use of X-rays became an established part of the medical profession. Since then, people have specialized in interpreting those images and writing medical reports summarizing their findings. One of the earliest radiology reports we know of was written by William James Morton of New York in 1896. It reads:

May 20, 1896. Dear Dr. Stieglitz,
The X ray shows plainly that there is no stone of an appreciable size in the kidney. The hip bones are shown & the lower ribs and lumbar vertebrae, but no calculus. The region of the kidneys is uniformly penetrated by the X-ray & there is no sign of an interception by any foreign body. I only got the negative today, and could not therefore report earlier. I will have a print made tomorrow. The picture is not so strong as I would like, but it is strong enough to differentiate the parts.
Yours sincerely,
William James Morton

Readers familiar with modern radiology reports might have noticed that the essence of the report has not changed much. Historically, the written report has played a large role in underlining that specialized skills were needed for interpreting those examinations. Consequently, most large academic hospitals soon had at least one full-time medical doctor devoted to reading imaging studies, and, thus, the profession of radiology was born.
What made (and makes) a great radiology report?
Early on, some radiologists stood out from the rest because of the structure, richness, detail, and/or complexity of the reports they crafted. One of them, Lewis Gregory Cole, a prominent New York ‘roentgenologist’, was well aware of the importance of pleasing his referring physicians, as well as their patients. He went to great lengths by typing cordial letters detailing his findings to the referring physicians. Alongside the letters, he included further documents containing photographic prints with additional highlighting and arrows explaining the points he mentioned in the report and background information and literature references. He then sent those materials in packages nicely wrapped with New York’s finest stationery — together with a second copy of the radiographs for the patient — to the referring physician.
Even though today’s radiology reports do not come wrapped in fancy stationery, radiology reports remain the “most important product that radiologists generate”. Never have radiology services been more in demand than they are today. Because of their central role within the healthcare system, radiologists are crucial elements in diagnosing and treating diseases and thus have touchpoints with all medical specialties, who depend on the timely communication of their findings via radiology reports.

While the report is one of the most critical of all the components of radiologists’ services, radiologists still receive surprisingly little guidance on how to write their reports during their formal training. Conventionally, the report is written in prose, and the writing skills and styles are learned on the job. There is no official standard, however, and the guidance available tends to be vague. For instance, one form of guidance that is often cited about reports is the Six C’s:
- Clear
- Correct
- Confidence level
- Concise
- Complete
- Consistent
These characteristics are supposed to make up a good report. There is no consensus, however, about what constitutes a ‘good’ report. So, it comes as no surprise that the reports vary within and among institutions as well as regions. Even the same radiologist might change their writing style to satisfy the preferences of different referring physicians.
To understand what makes a ‘good’ report, it is wise to consider the referring physicians, as they are the ones who request the radiologist’s services in the first place. Research suggests it is important to provide the referring physician with a “complete and accurate identification of relevant findings, a coherent opinion about the likely underlying cause of abnormalities and, if appropriate, guidance on further investigations that may add information or certainty.”

Challenges with free text reports
Poor radiology reports often fail to clearly communicate the radiologist’s findings to the referring physician and can delay the chosen treatment, potentially even leading to downstream medical errors. Because the reports most often employ a free text style, this can lead to ambiguity in the communication. Triple negations, vague prose, hedging, Kafkaesque sentences, and the redundancy of words are just a few aspects that can make it difficult to comprehend radiology reports. In addition, using speech recognition software can further alter the quality of the report. A survey by the American Healthcare Radiology Administrators (AHRA) found that one of the most frequent sources of complaints by referring physicians was poor structure and content. For instance, an analysis of reports on chest radiographs found up to 14 different terms being used to describe the same common abnormality.
Structured Reporting — many pros and some reservations

A structured report and the use of structured reporting templates can help address those issues. A 2017 study conducted by the European Congress of Radiology (ECR) showed that structured reports are helpful to referring physicians. Overall, the authors indicate that “it seems the more complex the study, the greater the benefit that you can yield from having a structured report.” It has been shown that structured reports are categorically more complete and effective than unstructured reports, with superior clarity, a perceived increase in clinical impact, better-facilitated information extraction, and improved surgical planning. Consequently, the American College of Radiology (ACR) concluded that structured reporting is the better reporting method, provided that structured reporting tools do not impede the radiologist’s productivity.
With the rise of a standardized lexicon for radiology and tools for integrating structured reports into DICOM format, we see a convergence of technology with the clinical need that is supposed to make structured reporting a usable reality, enabled by what is also known as ‘synoptic reporting’. The concept aims at producing machine-readable reports, directly from input data. In software like ‘Smart Reporting’, clinical data is tokenized when being input to the system, attached to whatever coding system you like (ICD-10, FHIR, SNOMED), and then processed into a free text report within a structured template.

Some of the reasons why structured reports have not yet superseded the free prose report are that writing and dictating are perceived still more time-efficient, giving radiologists a greater sense of freedom and flexibility using the traditional reporting model. Another repeated critique of structured reporting templates is their tendency to be disease-specific, while in routine reporting the disease might not be known at the beginning of the reporting process — even worse, focusing on the disease as the starting point of the reporting process might introduce dangerous bias and mislead radiologists to overlook other critical findings.
To address those challenges, new solutions following a ‘guided (structured) reporting’ approach have recently been introduced to the market such as ‘RadioReports’ by software company NeoQ — borrowing their template structure from the anatomical regions seen in a radiology image rather than being disease-specific.

Multimedia reports: a new era for radiology reporting?
Similar to reports by Lewis Gregory Cole, multimedia reports could provide added value to the referring physician. A multimedia report links various components — including hypertext, tables, graphs, and embedded images — into a single comprehensive report, making the report more informative. Plus, it has become possible to directly link the image with the text via hyperlinks. Research has shown the great clinical adoption of multimedia reports (with adoption rates in the clinical routine of up to 57% in less than two years), including a connection between the image and the radiology report using hyperlinks.

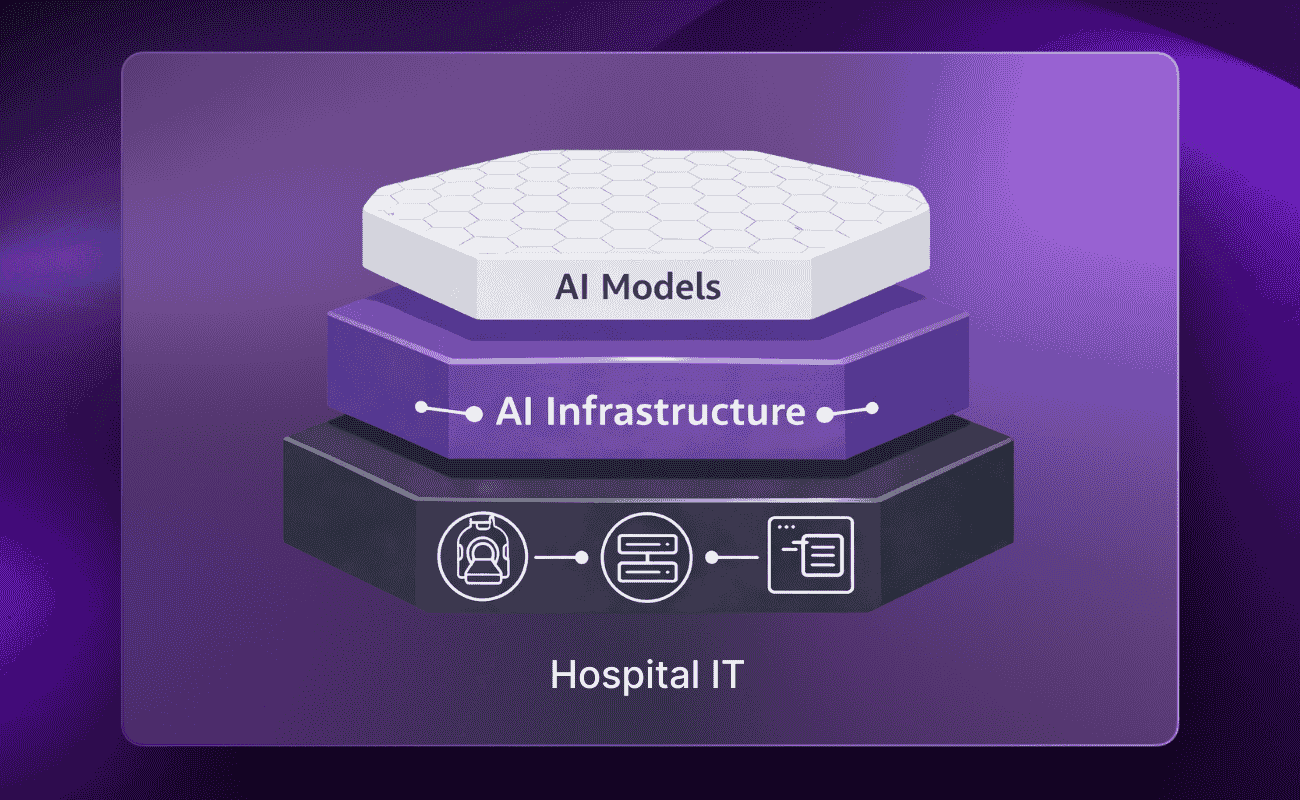
Furthermore, artificial intelligence entering the radiologist’s workflow can provide new inputs for such a new type of radiology report. Impossible reporting tasks or ones that required great effort — such as measuring the size and volume of different regions in the brain or comparing longitudinal changes between imaging studies over time — can now be done automatically by algorithms. Many new features will become available to radiologists as technology progresses.
The best out of all worlds
To sum up, we are listing a wishlist for the future of radiology reporting we have gathered in numerous conversations with radiologists, UX/UI designers, AI experts, and many other stakeholder groups, taking several aspects into account:
(1) Common data structure frameworks, e.g. for
- Capability of easy AI integration into the reporting process
- Statistical analyses of reporting data
- Transferability into different ontologies (RadLex → SNOMED, SNOMED → ICD-10, etc.)
- Automation of subsequent processes (e.g. billing)
- Other secondary usage scenarios of structured reporting data
(2) Homogenized reporting routine & guidelines (potentially facilitated by reporting templates), e.g. for
- Completeness
- Enhanced Readability
- Enhance Correctness
- Conciseness
- Clearness
(3) Flexibility, to account for
- Personal preference style
- Edge-cases that cannot be covered by ‘standard templates’
- Confidence Levels
(4) Multimedia Elements, to account for
- Consistency
- Interactiveness and Clearness
- Enhanced Readability
(5) Efficiency Gains (or at least not a Loss) & great UX, to account for
- ROI considerations
- Adoption
Epilogue — Sharing the radiology report: today and beyond

While there are still many printed-out reports that are sent to patients and radiologists via the mail or fax, the imaging study is often burnt onto a CD and handed over to the patient after the examination has been concluded. Only in the last few years have reports been more commonly shared digitally. Many countries and institutions, however, are still lacking the basic infrastructure to do so. As many developed countries are starting to invest heavily in such infrastructure, the written and printed reports might become, at some point, a relic of the past.


.png)
.png)

.png)
